Navigating India’s healthcare odyssey: from Ayushman Bharat to Universal Wellness
Preface
India is one of the world’s greatest economic triumph stories in recent times. Already overtaking China as the most populous country in the world, significant strides in India’s healthcare sector have been noticed in the last few years. However, India's economic growth and transition into a global leader with a $3 trillion economy have been accompanied by challenges in the social sector. While economic growth has been significant, it hasn't always translated into equitable improvements across various social indicators. India's Gini coefficient, a measure of income inequality, was 35.7 in 2019, indicating significant inequalities (According to World Bank data). The COVID-19 pandemic magnified the vulnerabilities and challenges within India's social sectors, particularly the healthcare sector. During the pandemic's peak in 2021, India faced severe shortages of hospital beds, oxygen supply, ventilators, and essential medical supplies. The healthcare system struggled to manage the sudden surge in cases, particularly in densely populated urban areas. In April 2021, India recorded one of the world's highest daily new COVID-19 cases, surpassing 400,000 points per day at its peak. The pandemic exposed the digital divide, as many people lacked access to telemedicine services for remote healthcare consultations.
The central government has undertaken numerous policies and brought in new frameworks to ensure that the population gets adequate access to quality healthcare services and bring in better infrastructural support and more unique cutting-edge technology, all aimed at ensuring that the disparities in healthcare facilities available across the country can be significantly minimized. A step in this direction was evident from the importance given to Universal Health Coverage (UHC), which was realized by introducing the Ayushman Bharat Yojana in 2018, which catered to all primary, secondary, and tertiary care.
The proposed National Health Protection Scheme (NHPS) replaced the existing schemes of the Government of India, namely the Rashtriya Swasthya Bima Yojana (RSBY) and the Senior Citizens Health Insurance Scheme (SCHIS). The NHPS eventually came to be known as PM-JAY. While the health and wellness centers (HWCs) aimed to deliver an expanded range of services close to the community, Pradhan Mantri Jan Arogya Yojana (PMJAY) primarily focused on providing secondary and tertiary care services to the underprivileged section of society.
The scenario of the Healthcare Sector in India and the initiation of the scheme
The current state of the Healthcare sector was marked by significant improvements in terms of life expectancy, infant mortality rate (IMR), and maternal mortality rate (MMR) due to increasing penetration of healthcare services across the country, extensive health campaigns, sanitation drives, increase in the number of government and private hospitals, improved knowledge of the importance of immunization, growing literacy rates, and other health indicators. The Indian healthcare sector is expected to rise three-fold, growing at a CAGR (Compound Annual Growth Rate) of 22% between 2016–22 to reach USD 372 billion in 2022 from USD 110 billion in 2016. In the Economic Survey of 2022, India’s public expenditure on healthcare stood at 2.1% of GDP in 2021-22 against 1.8% in 2020-21 and 1.3% in 2019-20.
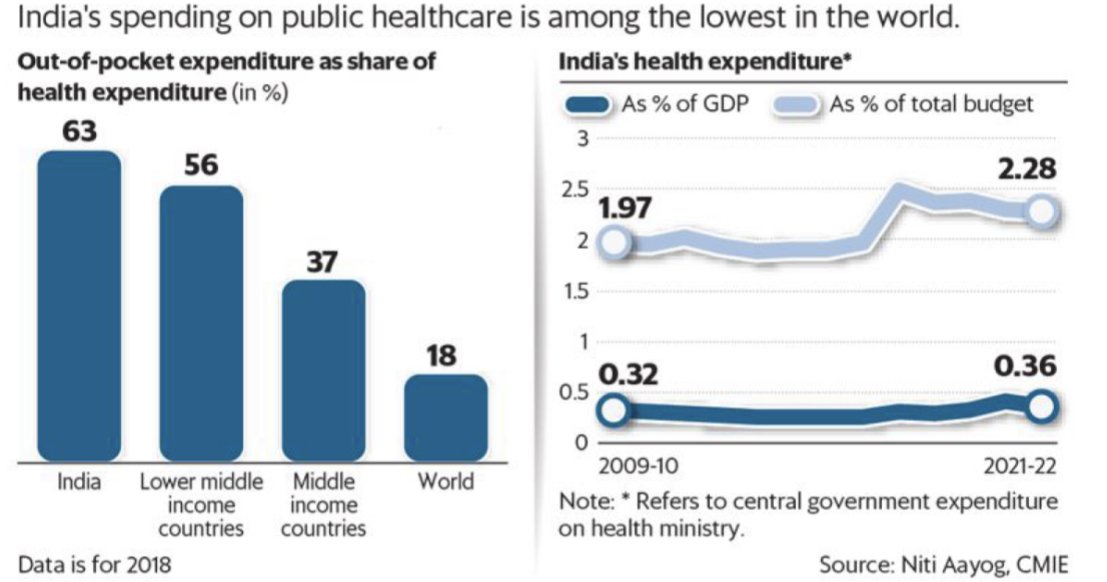
Yet the journey to becoming a state where public healthcare was at its highest potential is far from being realized, as the figure shows health expenditure as a percentage of total budgetary allocation (Data is for the year 2018).
India’s spending on the healthcare sector is among one of the lowest in the world. Primarily, a few areas needed to be taken into consideration
Skewed demand and supply of healthcare facilities(market being always significantly more).
India currently has 1.3 hospital beds per 1,000 population. There is also a shortage of skilled health workers, with 0.65 physicians per 1,000 people (the World Health Organisation standard is 1 per 1,000) and 1.3 nurses per 1,000 people. An additional 3 Million beds will be needed for India to achieve the target of 3 beds per 1,000 people by 2025. Further, another 1.54 Million doctors and 2.4 Million nurses will be required to meet the growing demand for healthcare in India. India will, therefore, need to increase the number of trained health personnel across various categories to achieve a ratio of at least 2.5 doctors and five nurses per 1,000 people by 2034. (Data from NITI Aayog, Investment Opportunities in India’s Healthcare Sector,2021)
Lack of penetration of healthcare schemes to the poorest of the poor.
An analysis of official data (data from the web portal of RSBY and individual state-level schemes) found that as of March 2016, the RSBY scheme could cover about 1.33 million families (a family of five members) - roughly 206 million persons. The RSBY, however, had the target to protect 70 million BPL families by the end of the Twelfth Five-Year Plan (2012–17). This shows that around 41% of the targeted families, consisting of many states, could not be covered under the scheme within the stipulated time. This reveals that the actual coverage under the scheme significantly falls short of the targeted families.
Changes in disease profiles and the need for newer technologies to combat these diseases meant a rising health expenditure.
Improvement in Health indices could only be sustained through a system of proper healthcare infrastructure (government and private hospitals and specialized health centers)and an adequate number of skilled healthcare workers, of whom India had a shortage compared to other countries.
The Rashtriya Swasthya Bima Yojana (RSBY), the predecessor to PM-JAY, was launched in 2008 and was managed under the Union Ministry of Labour. This scheme did reasonably well, reached almost all states, and got global recognition. As of September 2016, more than 41 million health cards (signifying enrolment in RSBY) had been issued, covering almost 150 million poor people, with nearly 460 districts participating. Although the share of eligible households enrolled in the program (enrolment ratio) was 57% nationally, there was considerable variation across districts(Data from the RSBY website). Providing a cover of Rs 30000/- per family per year, RSBY had its limitations. Also, rising Out-of-pocket (OPE) expenditures on health among the poorest and marginalized were a growing concern for the Government of India. Like any other massive scheme, RSBY had its hurdles and challenges. For instance, despite being functional for seven years, RSBY reached only 57% of its targeted benefits. Another intensely felt need was the gap in people's awareness and knowledge, and this was clearly because the Information, Education, and Communication (IEC) efforts needed to be stronger or more effective. A series of policy decisions and discussions led to the developing of a whole body of new ideas and immediate actions. RSBY was shifted from the Ministry of Labour to the Ministry of Health and Family Welfare (MoHFW) in 2015.
In 2016, the Ministry of Health and Family Welfare put together a small task force to initiate India's new health insurance scheme. After a few years of intensive effort in terms of early ideation and conceptualization, with the Union Budget of 2018, the government approved a Rs 5 lakh insurance cover scheme. The Union Cabinet, chaired by PM Modi, approved the Ayushman Bharat National Health Protection Scheme, later renamed PM-JAY, and expected to subsume the ongoing centrally sponsored schemes – the RSBY and SCHIS. A collaborative effort between the NITI Aayog and MoHFW, through the work of a small and dedicated expert group, led to the PM-JAY's initiation, and it is through these efforts that the insurance cover shifted from Rs 1 lakh to Rs 2 lakh and then finally to Rs 5 lakh.
Salient Features of the Scheme
The Government of India announced two significant initiatives in the health sector as part of Ayushman Bharat aimed at introducing path-breaking interventions to address the healthcare issue holistically in primary, secondary, and tertiary care systems, covering both prevention and promotion of healthcare technologies. The government of India envisioned that two health initiatives under Ayushman Bharat would build a New India 2022 and ensure enhanced productivity and well-being, prevent wage loss and financial hardship, create jobs, and boost the healthcare sector. The Indian healthcare system would take a great leap toward UHC. It was estimated that around 20 crores (80%) of families would be covered under AB-PMJAY, private insurance, and other government-funded health schemes such as Central Government Health Scheme(CGHS), Employment State Insurance Scheme (ESIS) and Ex-Servicemen Contributory Health Scheme(ECHS). The focus on providing comprehensive secondary and tertiary healthcare services under AB-PMJAY was further substantiated in the budget announcement on 5 July 2019, when the allocation for AB-PMJAY increased from INR 2,400 crore in FY 2018-19 to INR 6,400 crore for FY 2019-20; which saw 166.6 percent increase from the previous financial year.
AB-PMJAY is an entitlement-based scheme with no formal enrollment process and was targeted to cover around 10.74 crores out of the total targeted families - 8.20 crore families based in rural areas and 2.33 crore families based in urban areas. The latest Socio-Economic Caste Census (SECC) 2011 data was used to identify targeted poor, deprived rural families (D1, D2, D3, D4, D5, and D7) and 11 occupational categories of urban workers’ families. All such enrolled families under RSBY that do not feature in the targeted groups as per SECC data were included as well. States covering a much larger population than the AB PM-JAY beneficiary list were mandated to ensure that AB-PMJAY beneficiaries were mapped and covered by the conditions.
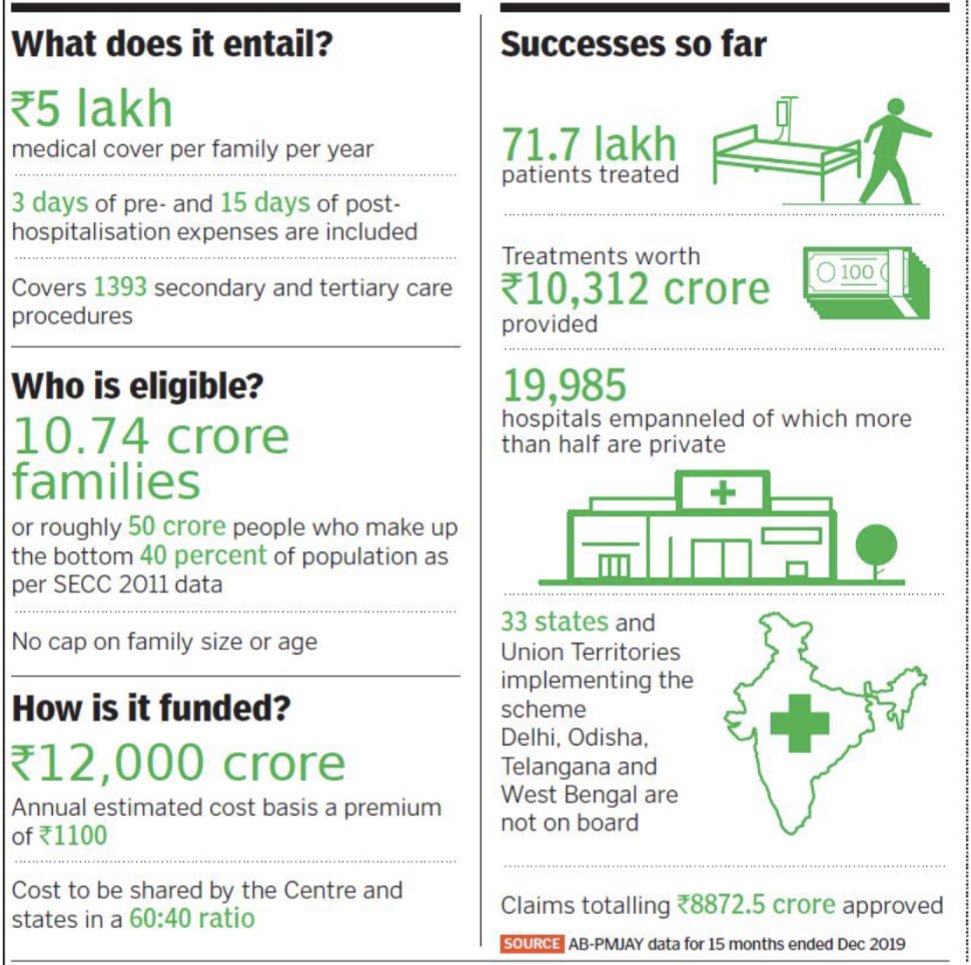
The salient features of the scheme promised certain benefits to the population of India and could be listed as follows and as shown in the figure
Establish 1.5 lakh health and wellness centers providing Comprehensive Primary Healthcare Services and covering approximately 10.7 crore families with INR 5 lakh annual coverage per family for secondary and tertiary care services.
Building Government institutional capacity by setting up National Health Authorities (NHA) at the Centre and State levels and making efforts to integrate the AB-PMJAY with existing state-level healthcare schemes(e.g., Rajiv Gandhi Jeevandayee Arogya Yojana set up in Maharashtra in 2010)
Enabling innovative business models, encouraging new market entrants, setting up economic hospitals across tier-II and tier-III, new PPP models, and significantly emphasizing strategic purchasing.
An increase in health coverage would potentially drive pharmaceutical and medical supplies demand as well as the demand for different kinds of medical equipment to implement the new healthcare infrastructure that would be brought in place.
Assessing the impact of COVID-19 on the AB-PMJAY Scheme
The COVID-19 pandemic and accompanying pan-India lockdown have significantly slowed AB PMJAY’s growth and uptake in several states. Different states, with varying experience levels and infrastructure for plan implementation, reacted to the pandemic differently. This change could be linked to more bottomless underlying supply, demand, and infrastructural set‐up factors. Surveys and discussions conducted across the country showed that providers faced financial and service delivery challenges from factors such as low utilization, delayed payments, inadequate and expensive supply of PPE, and with disruptions to the commodity supply chain. In contrast, beneficiaries faced physical barriers to access facilities even post‐lockdown, information asymmetry, and fear of contracting the virus at hospitals. AB PM-JAY aided the healthcare ecosystem by ensuring that the beneficiary registration procedure remained active and that impaneled institutions continued to deliver services to scheme beneficiaries. Under Ayushman Bharat, packages for ‘Testing for COVID-19’ and ‘Treatment of COVID-19’ were notified to treat COVID-19 patients in private hospitals. AB-PMJAY partnered with Uber India, an app-based taxi service, so patients and frontline workers could quickly be brought to the hospital. Without this scheme, mitigating the nationwide health crisis would have been impossible. Under PMJAY, many private hospitals were covered; 50% were personal, making them readily accessible to everyone. Many incentives were provided to private hospitals to facilitate the people in more efficient ways.
Conclusion
AB-PMJAY is gradually transitioning to an exponential phase after its incubation time, where it is being used to strengthen the capacities of hospitals, raising awareness and ensuring the effectiveness of the benefits provided under the scheme machinery.
A critical analysis of the scheme reveals that a lot is yet to be realized regarding the healthcare sector in India and its coverage under UHC, but this was a step in the right direction. The adjoining figure shows a few key statistics related to the scheme's implementation.
In June 2019, NHA signed an MoU with a CSR foundation of a banking group for capacity building of State and District personnel intending to provide training to more than 15,000 personnel over one year. It plans to develop an e-learning platform for systemic delivery and tracking of the learning process of various stakeholders. NHA also intends to leverage partnerships with developmental agencies, educational institutes, and other ministries for capacity building.
NHA has empaneled PSUs and National Healthcare Providers (NHCPs) under Ayushman Bharat by signing MoUs with organizations such as the Railway Board, Coal India, North Municipal Corporation, and New Delhi Municipal Council.
Provisioning of standardized care should be a key priority under Ayushman Bharat in the coming times. The diverse nature of empaneled healthcare providers may result in various treatment practices and clinical outcomes mainly due to the varied skills of the workforce, medical technologies, drugs and medical supplies used, and quality of infrastructure. In the recent past, MoHFW developed Standard Treatment Guidelines (STGs) for various diseases under the task force led by the National Health Systems Resource Centre (NHSRC) and other essential stakeholders like ICMR, DGHS, civil society organizations, academic institutions, and technical support of NICE, UK.
Efforts should be extended to encompass the remote regions of the country to help people extract the fruits of the scheme because it is seen that people living in such areas often remain unaware of such public sector initiatives. Public sector authorities should also be more vigilant towards the misuse of the scheme and ensure that adequate efforts are taken to protect and keep the records and patient and hospital data under the scheme confidential.
In pursuing transforming India's healthcare landscape, the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) stands as a commendable stride towards achieving Universal Health Coverage (UHC). This visionary initiative has attempted to bridge the gaps in healthcare access, aiming to provide comprehensive services to underprivileged populations. While the scheme's implementation has encountered challenges, its impact has been evident in improving health indices and creating a robust network of health and wellness centers. However, the journey towards realizing the full potential of UHC is ongoing. Strengthening healthcare infrastructure, addressing regional disparities, and ensuring the quality of care across diverse providers remain crucial The lessons from global UHC pioneers and the need for technological integration, effective communication, and continuous capacity-building should guide the future trajectory of AB-PMJAY. As India navigates the evolving healthcare landscape, the partnership between the government, the private sector, and communities will be pivotal. By aligning policies, harnessing innovation, and amplifying awareness, India's pursuit of equitable and accessible healthcare for all can evolve from a policy initiative to a resounding success story.
References
HRUBAJIT GOGOI, AMANISHA BORAH, ANISUR RAHMAN KAUSAR, ANTARA SAIKIA, DIPANKAR PARASAR. 2022. “Ayushman Bharat Pradhan Mantri-Jan Arogya Yojana And Its Crucial Impact On Human Health During The Time Of Covid-19 In India”. Journal of Pharmaceutical Negative Results, December 2850-56. https://doi.org/10.47750/pnr.2022.13.S10.341
https://www.india.gov.in/spotlight/ayushman-bharat-national-health-protection-mission
https://pmjay.gov.in/sites/default/files/2020-10/Assessing_Impact_of_COVID-19_on_PMJAY.pdf
Furtado, K.M., Raza, A., Mathur, D. et al. The trust and insurance models of healthcare purchasing in the Ayushman Bharat Pradhan Mantri Jan Arogya Yojana in India: early findings from case studies of two states. BMC Health Serv Res 22, 1056 (2022). https://doi.org/10.1186/s12913-022-08407-2
Dhaka, Rohit & Verma, Ramesh & Agrawal, Ginni & Kumar, Gopal. (2018). Ayushman Bharat Yojana: a memorable health initiative for Indians. International Journal Of Community Medicine And Public Health. 5. 3152. 10.18203/2394-6040.ijcmph20183043
NITI Aayog. (2021). Investment Opportunities in India's Healthcare Sector. NITI Aayog.https://www.niti.gov.in/sites/default/files/2021-03/InvestmentOpportunities_HealthcareSector_0.pdf
Institute for Studies in Industrial Development (ISID),. (2020, Dec). Penetration and coverage of government-funded health insurance schemes in India. Clinical Epidemiology and Global Health, 8(4), 1017-1033. https://doi.org/10.1016/j.cegh.2020.03.014
Written by Pratyasha Kar | Proofread by Yasmin Uzykanova